

6 (24%) also reported decreases in hearing.

There were minor problems in form of stitch abscesses or collections that were drained without removal of pack.īy 90 th day 4 (16%) cases reported better hearing up to 10-20 dB, and also minor increase (5 dB) in 9 (36%) patients, 11 (44%) patients did not report any improvement in hearing. There was no major complications reported intraoperatively as well as post operatively while in 2 (8%) cases, the post aural pack head to be removed due to formation of aural hematoma/abscess in 3(12%). As for the pathology 5 (20%) patients had frank cholesteatoma, 15 (60%) had granulations and 5 (20%) patients had both. Almost all patient gave h/o subjective decrease in hearing, 18 (72%) reported average gap 20-30 dB, while 7(28%) had an average gap of 30-40 dB. While 8 (32%) patients complained of the occurrence of dull earache, all patients complained of foul smell discharge, 13(52%) had h/o mucopurulent discharge while 21(84%) gave h/o scanty discharge. It was noted that majority of patients were in age group 11 to 20, i.e. The parameters for study included pain, discharge, granule extrusion, dizziness, epithelization rate, debris and other complications. The patients were followed up in the OPD on 15 th, 30 th, 45 th, 60 th, 90 th, 180 th day and then 6 months and 1 year post operatively. Final packing with ointment-impregnated gauze was done.Īll the patients were put on I/V, antibiotics, decongestants and painkillers in the post operative follow up for 10 days after which the pack was removed.
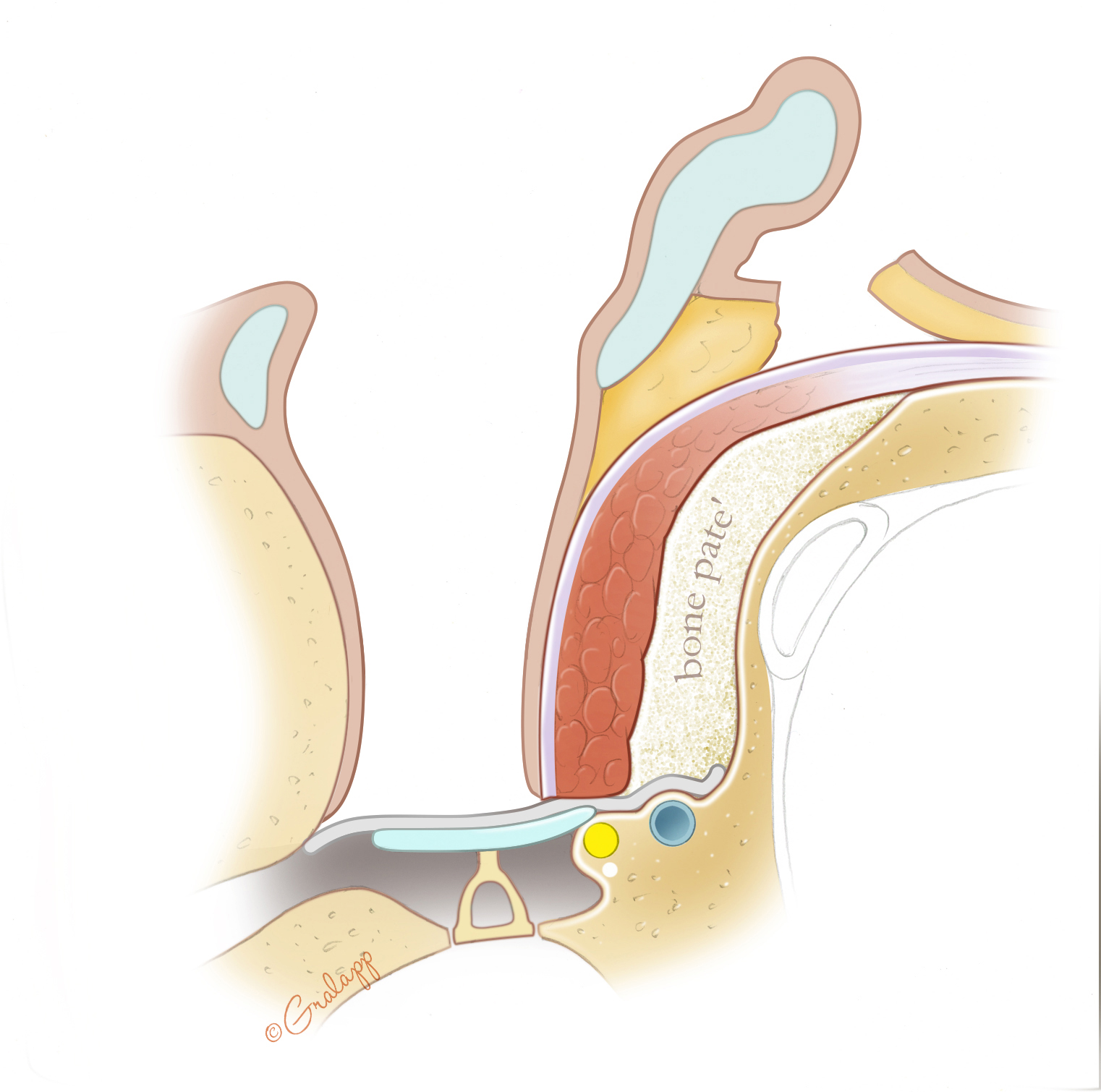
The inferiorly based periosteal flap was then rotated into the mastoid cavity to cover the granules and over it dry temporalis fascia was inserted to line the eardrum. Porous hydroxyapatite granules obtained by crushing commercially available hydroxyapatite blocks (0.5 > 1 cm) were dipped in antibiotic solution (Co-amoxyclav) for 10 minutes and then filled into the cavity completely and covering the lateral semi-circular canal. An inferiorly based periosteal flap was then devised near the tip of mastoid process.
#Mastoid obliteration trial#
© 2003 Otology & Neurotology, Inc.A randomized trial of 25 patients of either sex less than 60 years of age having atticoantral type of disease without any history of intracranial complication were included in the study.Īll the patients underwent initially modified radical mastoidectomy under general anaesthesia. Surgical techniques that include sterile harvest of the cranial bone graft mixed with antibiotic, revision of the cavity to expose viable native bone, inclusion of the epitympanic spaces in the obliteration, and complete coverage of the pÂte with autogenous fascia have proven critical to successful outcome. Mastoid obliteration with autogenous cranial bone is a safe and extremely effective option for treatment of problematic canal wall-down mastoid cavities. To date, no patient has required revision surgical intervention. For over 95% of patients, existing eustachian tube function has been adequate after obliteration. ResultsĬomplete take of the bony obliteration occurs in over 95% of cases 90% of treated patients enjoy complete absence of original symptoms, whereas symptoms improved in the remainder. Success of obliteration, incidence of symptoms prompting intervention, hearing outcome, incidence of recurrent cholesteatoma, and incidence of eustachian tube dysfunction necessitating treatment and need for revision surgical procedures. Transplanted autogenous cranial bone is used to induce osteoneogenesis resulting in complete obliteration of the epitympanic and mastoid spaces while maintaining a mesotympanic space. Thirty-six ears in 33 patients who underwent second-stage surgery for ossicular reconstruction during the same time period are also reviewed. Sixty-two ears in 56 sequential patients undergoing mastoid obliteration with major indications including recurrent infection, debris trapping in the canal wall-down cavity, intolerance of water exposure, calorically induced vertigo in an existing cavity, a semicircular canal fistula, and inability to wear a hearing device. To review the outcome in consecutive patients who have undergone complete epitympanic and mastoid obliteration and concurrent tympanic membrane reconstruction over a 53-month period.


 0 kommentar(er)
0 kommentar(er)
